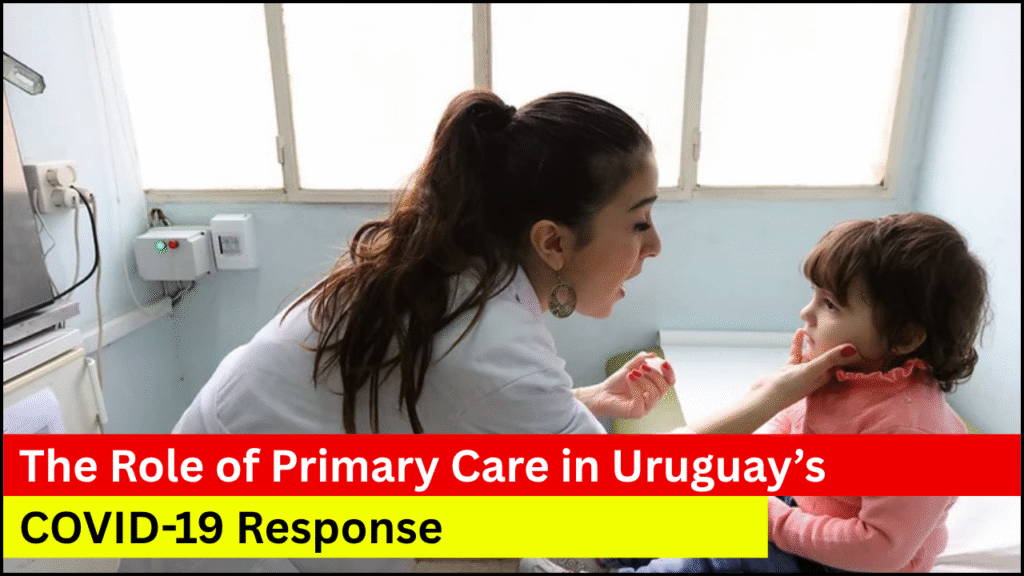
Uruguay’s COVID-19 strategy stood out in Latin America due to its efficient and decentralized health system. Primary care played a vital role in the country’s pandemic response by acting as the frontline of defense. Through a well-integrated network of community-based care, early detection, prevention strategies, and strong public health leadership, Uruguay managed to delay widespread outbreaks during the early phases of the pandemic. The country demonstrated how investment in strong primary healthcare can lead to more resilient outcomes during health crises.
Table of Contents
Key Components of Uruguay’s Primary Care Response
- Strong Public Health Infrastructure: A well-established public health system allowed Uruguay to integrate primary care with national emergency responses seamlessly.
- Decentralized Health Services: Community-level clinics provided localized care, ensuring continuity and early intervention.
- Multi-disciplinary Primary Care Teams: Family doctors, nurses, and community health workers collaborated to provide both clinical and preventive services.
- Effective Contact Tracing and Monitoring: Primary care centers were instrumental in active case finding and home-based patient monitoring.
- Equity-Driven Care Access: The government focused on reaching remote and vulnerable populations through mobile health units and rural health services.
Primary Care Strategies Implemented During the Pandemic
- Early Testing and Surveillance
- Primary care units facilitated rapid antigen testing across urban and rural zones.
- Symptomatic individuals were immediately evaluated by general practitioners at local centers.
- Telemedicine Services
- Introduction of teleconsultations to manage mild cases and reduce in-clinic exposure.
- Remote patient monitoring platforms were adopted for chronic patients and COVID-19 cases under home care.
- Public Health Messaging
- Primary care personnel played a crucial role in communicating safety protocols.
- Community education initiatives were deployed through local clinics.
- Continuity of Care for Non-COVID Patients
- Measures ensured treatment for patients with chronic conditions did not halt.
- Mental health services were incorporated into the primary care model to handle pandemic-induced stress.
Primary Care vs Hospital Care in Uruguay’s COVID-19 Management
| Aspect | Primary Care Approach | Hospital Care Approach |
|---|---|---|
| Patient Volume | Managed mild and moderate cases at local clinics | Treated severe and critical patients |
| Resource Use | Less resource-intensive, reliant on community health workers | High dependency on ICU beds, ventilators, and specialists |
| Accessibility | High, especially in remote regions | Limited, centralized in urban areas |
| Cost-Effectiveness | More cost-effective for large population outreach | More expensive and capacity-limited |
| Preventive Measures | Focused on education, mask distribution, and early screening | Focused on treatment and critical care |
| Patient Monitoring | Home visits, telehealth, follow-up through local clinics | In-hospital monitoring post-admission |
Role of Community Health Workers and Family Doctors
- Contact Tracing and Testing
- Community health workers conducted door-to-door symptom checks.
- Local practitioners coordinated neighborhood-based contact tracing efforts.
- Vaccine Roll-out Support
- Primary care centers assisted with organizing and administering vaccines.
- Mobile vaccine units targeted elderly and high-risk groups at their homes.
- Mental Health Support
- Trained staff provided counseling to individuals dealing with anxiety or isolation.
- Psycho-social support programs were embedded in community health routines.
Functions of Primary Care Teams During the Pandemic
| Team Member | Key Responsibilities |
|---|---|
| Family Doctors | Diagnosed patients, advised home care, escalated severe cases |
| Nurses | Conducted testing, administered vaccines, and monitored chronic conditions |
| Community Health Aides | Educated the public, supported contact tracing, and delivered medications |
| Social Workers | Linked patients with food, housing, and social aid programs |
| Mental Health Counselors | Provided emotional and psychological support to patients and families |
Collaboration Between Institutions and Primary Care
- Unified Health Response
- Public and private sectors collaborated under the Ministry of Public Health guidelines.
- Primary care was supported by central data systems that shared real-time case updates.
- Integrated Data and Communication Systems
- Patient tracking and digital records helped avoid overload in hospitals.
- Clinics received alerts about possible COVID-19 hotspots in their areas.
- Use of Local Networks
- Civil society and municipal councils worked closely with clinics to identify and assist high-risk populations.
Challenges Faced by Primary Care Providers
- Limited Resources in Rural Areas
- Some remote clinics lacked adequate protective equipment in the early phase.
- High Demand for Mental Health Services
- Surge in anxiety, domestic violence, and grief required more trained personnel.
- Fatigue Among Health Workers
- Extended hours and constant exposure to COVID-19 caused burnout.
- Digital Divide
- Telemedicine faced hurdles in areas with low internet penetration.
Strengths and Weaknesses of Uruguay’s Primary Care COVID-19 Response
| Category | Strengths | Weaknesses |
|---|---|---|
| Preparedness | Existing decentralized network of clinics | Limited stockpiles of PPE at the onset |
| Accessibility | Broad coverage even in remote communities | Telehealth is not accessible in all rural regions |
| Coordination | Strong link between public health and community care | Occasional overlaps in data reporting |
| Equity | Prioritized vulnerable groups for vaccine and care delivery | Some underserved populations still faced logistical barriers |
| Mental Health | Integrated into primary care through community initiatives | Limited number of trained mental health professionals |
Lessons Learned and Innovations for the Future
- Decentralized Systems Work in Crises
- Empowering local health centers ensures faster, culturally sensitive responses.
- Telemedicine Requires Investment
- Broader internet access and digital literacy programs are essential.
- Community Health Workers are Indispensable
- Future public health strategies should include upskilling and career development.
- Mental Health Integration is a Priority
- Psychological care should be made a permanent fixture in primary health.
Looking Ahead
Uruguay’s response to COVID-19 proves that strong primary care systems can serve as the foundation of an effective national health strategy. Community-based care, early intervention, and equitable health delivery helped the country delay the worst impacts of the pandemic. By integrating mental health support, leveraging local knowledge, and emphasizing decentralized access, Uruguay showed how thoughtful, people-centered primary care can be a model for managing global health crises. Future reforms should aim to reinforce these structures and extend their resilience for upcoming challenges.